
Ageing well
This section considers the health and wellbeing of adults in the so-called third age, retirement, older age, as well as the end of life.
According to the 2021 Census, York is home to 38,734 people over the age of 65, nearly a fifth of the total York population. Haxby and Wigginton ward has the highest number of older people with 4,658 residents. Fulford ward, with a total of 1,037 older residents, has the lowest representation.
It's now expected that people nationally will live longer lives than previous generations. But how do we ensure that senior members of society are living as healthy and active lives as possible? The information below provides key insights into the areas concerning advancing age, and also where York is performing well and areas that need to be reviewed.
C
Care in the Community
Social care generally refers to additional support and professional care that may be required to enable people to live comfortably. This can include homecare, home adaptations, specialist housing, or residential care. Maintaining independence whilst receiving support to manage daily tasks in an important factor for good health and wellbeing. In York, adult social care users are generally satisfied with the care and support services offered with 71.1% stating they have control over their daily lives. This is similar to national rates of adult social care users who are generally satisfied with the care and support services offered.
Where needs become more complex, a permanent move to residential care may be necessary. Nursing care homes offer an important and essential service for some elderly people, but a population with a high use of care homes can indicate a reliance on adult social care services and missed opportunities to reduce or delay frailty or illness in older adults. York has a similar proportion of over 65-year-olds living permanently in residential nursing care to the national average, and the majority of York's statistical neighbours. As of 2021, care home beds per 100 people aged 75 years plus was 8.6 in York (9.4 out of 100 nationally). Nursing home beds per 100 people aged 75 years plus was 4.5 in York (4.6 out of 100 nationally).
COVID-19 Pandemic
The COVID-19 pandemic is a global outbreak of infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). It was declared a Public Health Emergency of International Concern (PHEIC) on 30 January 2020, and later a pandemic on 11 March 2020. Since 5 May 2023, the World Health Organization (WHO) confirmed it no longer fit the definition of a PHEIC. York was unlike other places in the UK and globally. As of January 2024, there have been a cumulative rate of 35,677 cases per 100,000 residents in York. Nationally, this is 37,178 per 100,000 people. The majority of deaths from COVID-19 were recorded in people aged 75 years and over (Coronavirus Data (Restricted Access)).
D
Deaths from communicable disease
Prior to the COVID-19 pandemic, illnesses that spread from person to person were the cause of a relatively small number of deaths in the UK, particularly in comparison to other countries. The significant effort given to the monitoring, identification, vaccination and treatment of infectious conditions continues for other diseases, such as influenza and norovirus. The number of deaths from communicable disease is one indicator that helps to measure the impact of interventions. Over the past few years, York has had lower rates of death from communicable disease than both the regional average and the majority of York' statistical neighbours. Over the last 10 years, York's rates of death from communicable disease has been similar to or lower than the national average.
Dementia diagnosis
An accurate and timely diagnosis of dementia is the first step to getting the right help and support. The recorded prevalence of dementia in York is lower than both regional and national rates. This does not necessarily mean there are fewer people living with dementia and is does not include people who are yet to receive a diagnosis.
There are different measures to look at when reviewing provision of dementia services in York.
Estimated diagnosis rate in people aged 65 years and over
The diagnosis rate is calculated by dividing the number of people with a dementia diagnosis by the total estimated number of people living with dementia. In 2023, this rate was statistically worse than rates in England. However, data from the other 4 years shows that York rates of diagnosis are significantly below the national average at 56.1%.
Dementia prevalence in people aged 65 years and over
Prevalence measures the number of people currently living with a disease at a certain point in time. At present, the recorded prevalence is 3.48% which is lower than the national and regional prevalence.
Crude Recorded Prevalence of dementia in people aged under 65 years
Dementia in people younger than 65 is extremely rare. Often referred to as early-onset dementia, people with this diagnosis are likely to have more unusual variants such as fronto-temporal dementia and Korsakoff's syndrome which is related to alcohol. Their circumstances are generally very different to older people living with dementia- most are in employment, have young families, and do not have other comorbidities.
In York, the crude recorded prevalence of dementia in this cohort is very similar to the national average. In 2020, this count was measured at 2.37 per 10,000 people compared with 3.05 per 10,000 nationally.
Dementia Care Plans reviewed in last 12 Months
York data has mirrored national trends. In 2020 and 2021 39.4% of dementia care were reviewed annual. This is a significant decrease from 2017 to 2019 when approximately 75% had a 12-month review. As this change has also been observed nationally it is likely that the COVID-19 pandemic was a considerable contributor.
E
Emergency hospital admissions for falls
Falls are the largest cause of emergency admission to hospital in older adults, and a common factor that triggers a permanent move to nursing home care. Emergency hospital admissions for falls in York are statistically similar to regional and national averages with lower numbers reported when looking at admissions for people aged 65 to 79 years.
Chart showing the number of emergency hospital admissions due to falls
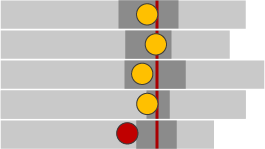
The above graph shows the proportion of falls occurring across England. The:
- yellow circle indicates the number of falls is similar to the England average
- red circle indicates the number of falls is significantly higher or worst than the England average
- red line indicates the mean average number of falls
| Row in the graph | Indicator | Period | Count in York | Value in York | Region in England value 1 | Region in England value 2 |
|---|---|---|---|---|---|---|
| 1 | Emergency hospital admissions due to falls in people aged 65 and over | 2021 to 2022 | 855 | 2,065 | 1,901 | 2,100 |
| 2 | Emergency hospital admissions due to falls in people aged 65 to 79 | 2021 to 2022 | 230 | 819 | 879 | 993 |
| 3 | Emergency hospital admissions due to falls in people aged 80 plus | 2021 to 2022 | 625 | 5,676 | 4,866 | 5,311 |
| 4 | Emergency hospital admissions due to falls from furniture (aged 0 to 4 years) | 2016 and 2017 to 2020 and 2021 | 70 | 143.0 | 120.4 | 123.1 |
| 5 | Emergency admissions due to falls in children aged 0 to 4 | 2018 and 2019 to 2020 and 2021 | 160 | 557.7 | 431.3 | 428.6 |
Overall, emergency admissions for falls in children aged 0 to 4 in the periods 2018 to 2019 and 2020 to 2021 have the worst average for falls whereas emergency hospital admissions due to falls in people aged 65 to 79 in the period 2021 to 2022 were statistically better than average.
Emergency hospital admissions due to falls in people aged 65 and over, 80 plus and emergency hospital admissions due to falls from furniture in children aged 0 to 4 were about average across England.
H
Healthy life expectancy
Healthy life expectancy is a measure of how many years of life a person can expect to be in good health for. It is a useful indicator to understand the health of older adults and how a population will experience older age, as well as the potential need for health and social care support. In York, males born in 2024 can expect to have a health life expectancy of 65.3 years which is significantly higher than the national average of 63.1 years. Girls born in 2024 have an average healthy life expectancy of 64.6 years which is statistically similar to the national average of 63.9 years.
L
Life expectancy at 65
This is an indicator of how many more years a person will live, on average, after they reach the age of 65. In 2021, both men and woman in York were likely to live longer than nationally; the life expectancy of women at 65 is 21.8 additional years (nationally 21.0 years), for men 19.1 additional years (nationally 18.4 years). In both instances, York residents were only second to North Yorkshire in living longer.
Q
Quality of life
Quality of life is defined by the standards of health, happiness and comfort experienced by an individual. The most recent quality of life assessment in 2016 and 2017 looked at the level of practical limitations to everyday activities experienced by a person. The health-related quality of life reported by residents in York who are aged 65 or over is higher than the national average. This is a stable trend, with older residents in York consistently reporting higher health related quality of life for at least the last 5 years.
Health related quality of life for older people 2016 to 2017
| Area | Value | 95% lowe CL | 95% Upper CL |
|---|---|---|---|
| England | 0.735 | 0.734 | 0.736 |
| Yorkshire and the Humber region | 0.731 | 0.728 | 0.734 |
| York | 0.778 | 0.757 | 0.799 |
| North Yorkshire City | 0.766 | 0.759 | 0.773 |
| East Riding of Yorkshire | 0.754 | 0.744 | 0.765 |
| Calderdale | 0.752 | 0.737 | 0.767 |
| Leeds | 0.741 | 0.733 | 0.749 |
| Kirklees | 0.740 | 0.730 | 0.750 |
| North East Lincolnshire | 0.735 | 0.720 | 0.749 |
| North Lincolnshire | 0.734 | 0.716 | 0.751 |
| Sheffield | 0.724 | 0.715 | 0.733 |
| Bradford | 0.718 | 0.706 | 0.729 |
| Rotherham | 0.714 | 0.699 | 0.728 |
| Doncaster | 0.713 | 0.701 | 0.725 |
| Wakefield | 0.702 | 0.688 | 0.715 |
| Kingston Upon Hull | 0.697 | 0.684 | 0.711 |
| Barnsley | 0.676 | 0.661 | 0.691 |
The graph shows the value of health related quality of life for older people in 2016 and 2017. People were asked to rate their quality of life out of 10 with the graph demonstrating these score as a decimal.
- England is set as the comparator and is demonstrated by the grey bar at the top of the chart
- Yorkshire and Humber collectively is also rated just below the England bar
- The green bar indicates those areas where people rated their quality of life as significantly higher than the England average
- The yellow bar indicates those areas where people rated their quality of life as similar to the England average an average
- The red bar indicates those areas where people rated their quality of life as significantly lower than the England average
The following areas were indicated as having higher quality of life scores for older people than nationally:
- York
- North Yorkshire City
- East Riding of Yorkshire
- Calderdale
The following areas were indicated as having quality of life scores that were similar to national scores:
- Leeds
- Kirklees
- North East Lincolnshire
- North Lincolnshire
The following areas where older people rated their quality of life as significantly lower than in England were:
- Sheffield
- Bradford
- Rotherham
- Doncaster
- Wakefield
- Kingston Upon Hull
- Barnsley
Overall, Yorkshire and Humber had lower quality of life scores for older people than in England. This was particularly observed in urban areas where there were statistically higher levels of deprivation than in other areas of Yorkshire & Humber.
R
Reablement services
Reablement services are offered to older adults upon leaving hospital and where there is an increased risk that they will be readmitted to hospital in the days, weeks and months that follow. They are intended to support people to move back home after a hospital stay and to prevent avoidable returns to hospital. In York, fewer than 1% of people aged 65 years and over were offered reablement services upon being discharged from hospital. This is much lower than the England average of 2.8%.
S
Screening
Screening is a way of identifying people with an increased risk of a particular condition. They may not have any symptoms and could be otherwise healthy. There are a range of tests offered by the NHS to different groups of people. Screening programmes are optional for people to attend and include the following for older people:
- Abdominal aortic aneurysm (AAA) screening
- Breast screening
- Bowel cancer
- Cervical screening
- Diabetic eye screening
Overall, screening rates are either statistically similar or higher than the national and regional averages with the exception observed in rates of AAA screening. York has the second lowest rate with fewer than 40% attending screening.